The formation of a complete organ such as the heart requires that different types of cells assemble and become organised in a specific way. If the maturation and migration of these cells are disrupted, congenital cardiac malformations can occur, the most common birth defects. Yet the processes governing how each cell type moves into the right place at the right time have largely been a mystery.
A new study published in the scientific journal Nature reveals molecular factors that determine the fate of specific cardiac stem cells and exposes mechanisms of disrupted cardiac development. This study provides a new framework for investigating congenital heart defects. These results stem from a close collaboration between researchers of the Luxembourg Centre for Systems Biomedicine (LCSB) of the University of Luxembourg, the Gladstone Institutes in California and CIC bioGUNE. While the American team provided experimental expertise and in vivo validation, the LCSB group made use of its long-standing know-how for computational modelling of complex networks.
In order to study these processes, the researchers first had to discern the role of tens of thousands of cells during formation of the heart. It is an essential step to determine how genetic mutations can cause birth defects. Gladstone President and Senior Investigator Deepak Srivastava and his team were able to compile a catalogue containing all the genes that are active during different stages of heart development and identifying the cells in which they can be found. Once they identified the numerous types of cells involved in heart development, the researchers wanted to learn how these diverse cell types are generated. To do so, they teamed up with computational biologists at the LCSB who specialise in uncovering the molecular drivers leading toward different cell types.
“Our group has a long history of developing computational models to understand cell conversion. We have the expertise to study whole networks of molecular factors that control cell identity,” explained Prof. Antonio Del Sol, head of the Computational Biology group at the LCSB and Ikerbasque Research Professor at the Research Center CIC bioGUNE in Bilbao (Spain). “When we joined the project, we applied our method to predict – without any kind of prior knowledge – which factors govern the fate of the different cardiac cells.”
The computational analysis performed by the Luxembourg researchers successfully predicted which molecular factors are involved in generating specific cell types in the heart. It especially identified a major player, called Hand2, as important for the specification of cells of the outflow tract, the structure where major outgoing blood vessels of the heart arise. Whereas in lab conditions mice lacking Hand2 failed to form the right ventricle, which pumps blood to the lungs, the new prediction made by the Luxembourg researchers suggested that Hand2 is not required for cells being instructed to grow into right ventricular cells. Instead the computational model predicted that Hand2 is critical in forming the cells of the outflow tract. This unexpected result triggered new experiments to resolve the discrepancy between the computational analysis and previous in vivo observations. The prediction turned out to be correct, highlighting the accuracy of the computational model.
These results revealed the mechanisms by which the disruption of the fate of a few cells during development lead to defects in the formation of the heart. On top of providing a new framework for investigating congenital heart defects, they could open avenues towards the implementation of cell therapy. “We were able to show that, with our model, it is possible to identify the factors that are essential for the differentiation of specific cardiac cells,” explained Antonio Del Sol.
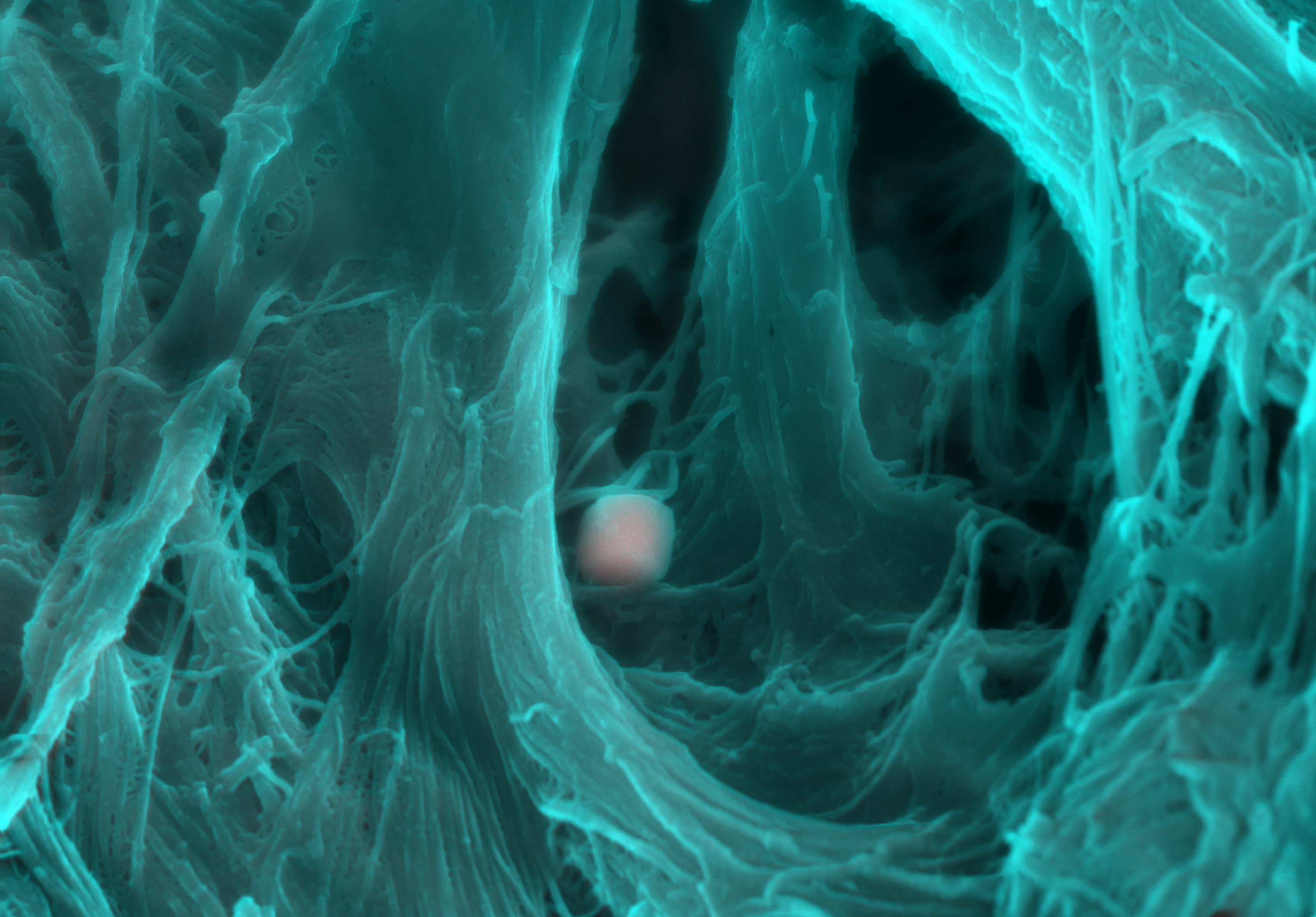
.png)
